There are no items in your cart
Add More
Add More
| Item Details | Price | ||
|---|---|---|---|
In the dentistry practice, medical emergencies can develop anytime. From sudden allergic reactions to cardiovascular incidents, being well-versed in emergency protocols and having access to essential emergency drugs can significantly affect patient outcomes. Hence, dentists must be prepared for unexpected situations and equipped with the knowledge to handle medical emergencies effectively.
This blog will delve into emergency dentistry, focusing on the critical aspects of managing medical emergencies within a dental office. Whether it's understanding the signs and symptoms of a dental emergency or knowing how to handle a patient in distress, we aim to equip you with the knowledge and skills needed to navigate these critical situations confidently.
An emergency is a medical condition that needs urgent care. Every Dental clinic does experience a dental emergency. Every dentist must be able to identify, assess, and manage a potentially life-threatening situation until the patient can be taken to a hospital.
Understanding pathophysiologic processes and how to correct them is essential for successful patient treatment. Even in hospitals with the best supervision, witness some emergencies end in disaster. People have heart attacks daily and they might be in your office at the time. You must know what to do to give the patient the best chance of healing.
To ensure the safety of patients and effectively manage medical emergencies in the dental office, several preventive measures, training, and the availability of equipment and drugs are crucial. Maintaining comprehensive medical history records and regular updates is essential for all patients, with particular attention given to those with severe medical conditions. Patients with unstable conditions may need to refer a dental hospital.
Staff members should undergo proper training to be well-prepared and knowledgeable about emergency protocols, with clearly defined roles. It is vital to have a readily available Emergency Drug Kit and a thorough understanding of its correct usage. Furthermore, dental clinics must ensure that their equipment and drugs are up-to-date, easily accessible, and regularly checked for proper functioning. These measures allow dental practices to be fully prepared for any unforeseen medical situation.
All patients must have thorough medical histories documented, which must be updated often. Patients with serious medical issues should be evaluated to see if they are suitable for dental treatment. Referrals for treatment at a dental hospital should be made for patients with severe or unstable medical conditions.
A dental clinic's employees should be educated to handle medical emergencies, and a collaborative approach should be encouraged. There should be protocols, so employees know their responsibilities in handling emergencies. Although it's essential to have a portable emergency drug kit, it's even more important to be ready to follow the correct emergency procedures and administer the medications properly.
Get trained, run mock drills, and practice frequently to be effective. Understand the fundamentals of recording and evaluating vital statistics, the ABCs of resuscitation, how to provide oxygen intramuscularly, and when appropriate, where intravenous medication distribution is needed. It is necessary to enrol in training and certificate programs for the same.
Drugs and emergency equipment must be readily available and in good working order. They should be saved for easy identification. The equipment must be tested regularly to ensure they are fit for operational purposes.
In dental practices, the following equipment must be carried and immediately available:
Drugs | Indication | Initial Adult Dose |
Oxygen | Almost any medical emergency | 100% inhalation |
Epinephrine | Anaphylaxis. Aasthma unresponsive to albuterol/ salbutamol. Cardiac arrest. | 0.1 mg IV or 0.3-0.5mg IM. 0.1 mg IV or 0.3-0.5mg IM. 1.0 mg IV. |
Nitroglycerin | Angina pain | 0.3-0.4mg sublingual |
Antihistamine (dephenhydramine or chorpheniramine) | Allergic relations | 25-50mg IV, IM. 10-20mg IV, IM |
Albuterol/salbutamol | Asthmatic bronchospasm | 2sprays: inhalation |
Aspirin | Myocardial infraction | 160-325 mg. |
Drugs | Indication | Initial Adult Dose |
Glucagon | hypoglycemia in unconscious patient | 1 mg IV or IM. |
Atropine | clinically significant bradycardia | 0.5 mg IV or IM. |
Ephedrine | clinically significant hypotension | 5 mg IV or 10-25 mg IM. |
Hydrocortisone | adrenal insufficiency recurrent anaphylaxis | 100 mg IV or IM. 100 mg IV or IM. |
Morphine and nitrous oxide | angina-like pain unresponsive to nitroglycerin | tritate 2 mg IV, 5 mg IM ~35%, inhalation. |
Lorazepam or Miodazolam | status epilepticus | 4 mg IM or IV. 5 mg IM or IV. |
Flumazenil | benzodiazepine overdose | 0.1 mg IV. |
Common Reaction to the unconscious patient
Despite the wide range of potential causes, the first assessment and therapy of an unconscious or collapsed patient follow a similar pattern. The use of drugs, trauma, or deteriorating medical conditions can all result in unconsciousness. Nevertheless, the most typical reasons for losing consciousness include:
Vasovagal Attack | It is generally associated with anxiety. Premonitory signs of faintness include chilly, clammy skin, pallor, initially bradycardia and a low pulse, then tachycardia and a full pulse; however, they are not always present. Recuperating quickly while supine or with their heads slightly bowed (a maximum recommended tilt of 10 degrees). |
Hypoglycemia | This is commonly observed in starved patients or diabetics with insulin overdose caused by stress or starvation. Rapid recovery after oral glucose administration or, if unconscious, glucagons followed by oral glucose upon regaining consciousness. |
Steriod Crisis | Only seen in those who are taking systemic steroids as a result of stress. |
Cardiac Arrest | There is no centre pulse. Typically, there is a history of angina, coronary artery disease, hypertension, or other risk factors. |
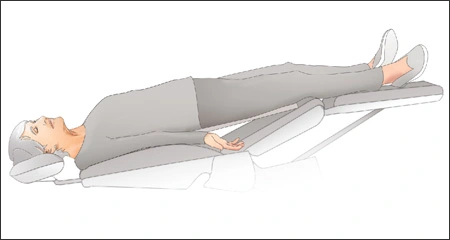
With up to 2% of patients experiencing syncopeprior to or during dental treatment, it is the most prevalent cause of unexpected loss of consciousness. The likelihood of vasovagal syncope while under GA, and thus failing to recognize and rectify cerebral hypoxia, is the primary rationale for advocating the supine posture. Predisposing factors for fainting are Pain; Anxiety; Fatigue; Relative hyperthermia; Fasting.
Signs and Symptoms
Differential Diagnosis
A faint can mimic far more severe disorders, several of which can be ruled out by reviewing the patient's medical history. Strokes, corticosteroid deficiency, medication responses and combinations, epileptic fit, hypoglycemia, and MI are examples.
Prevention and Management
Diagnosis and Management
For a cardiac arrest diagnosis, the patient must have:
Place your patient’s hand on the patient's neck to feel the carotid pulse.
Protocol/Basic Life Support
A patient's history of corticosteroid use collapses.
Corticosteroids reduce the adrenal response to stress in a therapeutic manner. This is more likely to occur during treatment and at a larger dose.
The primary goal is to prevent stress-induced collapse; if the patient has had steroids in the last year or is currently on steroids, cover any stressful procedure, anaesthesia, infection, or episode of trauma with 100 mg hydrocortisone 1M 30 minutes before intentional stress.
It is a misconception to suppose that avoiding prophylactic steroids reduces the likelihood of undesirable steroid effects.
Doubling the oral dose may help, but it is hit or miss. Calculating a 'precise' dose is overly complex. Unless you have a compelling cause to change, prescribe 100 mg hydrocortisone 1M.
Symptoms and Signs
Patients in acute pain should be treated as soon as possible. If such a patient collapses, the diagnosis is established by pallor, a quick, weak pulse, a profound and sudden drop in blood pressure, and loss of consciousness.
Management
Position yourself supine. Keep the airway open. Give O2. Obtain urgent IV access to 500 mg hydrocortisone. Ensure that assistance (such as an ambulance) is requested. Other possible reasons for collapse should be ruled out.
It is important to remember that penicillins and cephalosporins have a 10% cross-over in an allergic response. An anaphylactic reaction is not an all-or-nothing event, and there are many levels of severity. The reaction usually begins a few minutes after a parenteral injection rather than immediately. However, some caution should be exercised because the faster an anaphylactic reaction starts, the more severe it is likely to be.
Symptoms include flushing, itching, numbness, cold extremities, nausea, and occasionally abdominal pain.
Signs:
Wheezing, face puffiness, rash, and chilly, clammy skin with a thin thready pulse are among the symptoms. A loss of consciousness and extreme pallor may evolve into cyanosis when respiratory failure develops.

Diagnosis differentiation:
When an asthmatic is given an NSAID to which they are allergic, it might be challenging to distinguish anaphylaxis from acute asthma. Adrenaline has bronchodilating properties. Angioedema appears suddenly, with significant facial and neck allergic swelling. The airway is in danger and should be treated as if it were anaphylactic. Don't worry; go through acute asthma before beginning anaphylactic management.
Management:
Allow the patient to breathe in the most comfortable position possible while administering oxygen (5 litres per minute) through a facemask. The medications are administered in the following order:
Fits in a known epileptic may be triggered by malnutrition, flashing lights, certain medicines such as tricyclics, methohexitone or alcohol, or menstruation; they may also occur after a deep faint. Most epileptic fits do not require active intervention because the patient typically recovers independently. Careful placement is required to keep the patient from injuring himself.
Signs and Symptoms
Trauma, a malignancy, or alcohol withdrawal could cause the fit. A first fit in an adult should be thoroughly investigated.
Status Epilepticus
If the fit occurs again, the patient has entered the state of status epilepticus. This is an emergency that requires immediate attention.
Management
Hypoglycemia is a diabetic emergency that can arise before seeing the dentist. It is a severe and sometimes fatal diabetic complication caused by a missed meal, excess insulin, or increased calorific requirement due to activity or stress. Most diabetics are skilled at detecting the onset of hypoglycemia; nevertheless, some may lose this ability, especially if switching from porcine to human insulin. It is critical to recognize this state, and an acutely collapsing diabetic should be deemed hypoglycemic until shown differently, such as by "BM" sticks or blood-glucose readings.
Diagnosis
In a diabetic, disorientation, irritability, increased sleepiness, excitability, or violence indicate hypoglycemia. They frequently look to be inebriated.
Management
Exposure to an allergen can cause an acute asthmatic episode in a patient prone to bronchospasm. Cold, activity, or anxiety can all cause an infection.
Symptoms and Signs
Management
Use the patient's anti-asthmatic medications, such as salbutamol inhalers. This should ideally be delivered through a nebuliser.
A do-it-yourself nebuliser can be made by inserting the patient's inhaler into the bottom of a paper cup. When the inhaler plunger is depressed repeatedly, an aerosol is created inside the cup that the patient can inhale. Most reversible airway obstructions will be relieved. Steroids should be given as oral prednisolone if the patient has it on hand or as IV hydrocortisone up to 200 mg IV.
However, combining salbutamol, steroids, and O2 will typically completely resolve an attack. Only partially responsive patients must have underlying irritants like a chest infection either ruled out or addressed. Individuals who do not respond require urgent hospital admission.
Keep in mind that anaphylaxis might mimic acute asthma.
Remember to use 0.5 mL of adrenaline 1:1000 s.c.
Management in dental practice:
Maintain the patient's upright position. Oxygen should be administered. Use an inhaler or a nebulizer to provide salbutamol. Steroids should be administered.
If the patient responds ultimately, allowing them to return home is fair. If there is any question, take the patient to the nearest emergency room.
Many dental treatments include the use of delicate equipment and the supine position of patients, which increases the danger of a patient breathing a foreign body. There are two possible outcomes. Depending on whether the item hits the upper or lower airway.
Upper Airways
A choking patient should be bent forward to facilitate coughing. It will set off the cough reflex. It may clear the impediment.
If the obstruction is complete or cyanosis is present,
Conscious Patients:
Unconscious Patients:
Lower Airways
The condition will be less severe because only a part of the lungs will be obstructed. It is also simpler to overlook. Traditionally, this entails a tooth or tooth fragment falling off the forceps and being inhaled, with the object ending up in the right posterior basal lobe while the patient is semi-upright. If this occurs, notify the patient and schedule a chest radiograph as soon as possible. If the offending item is in the lungs, a chest physician should remove it using fibre-optic bronchoscopy, which will eventually cause collapse and infection distal to the obstruction. Lobectomy is only used in rare cases.
In conclusion, managing medical emergencies in the dental office is of utmost importance to ensure patient safety and positive outcomes. Dentists must be well-prepared and equipped with the knowledge and skills to handle unexpected situations effectively. Prioritizing patient safety and understanding pathophysiologic processes are essential for successful treatment. Preventive measures, comprehensive medical history records, and staff training are crucial in emergency preparedness. The availability of emergency equipment and drugs, along with their proper maintenance, is vital. Recognizing common medical emergencies such as unconsciousness, fainting, cardiac arrest, anaphylactic shock, and epilepsy is essential for prompt and appropriate management. By being proactive and well-trained, dental professionals can confidently navigate medical emergencies and provide optimal patient care.
Enroll to docMEP’s Basics of Exodontia Online Video lecture Series to learn Clinical Tips about the Steps for interalveolar and trans alveolar extraction and possible complications that a dentist may encounter in the clinical practice.